Blog | Aug. 30, 2023
MRD in AML: the next step in fighting leukemia
Evidence for “liquid biopsy” in clinical oncology continues to increase. Clinical practice guidelines now recommend plasma analysis alongside, and in specific situations in place of tumor tissue (references 1, 2). With the introduction of diverse new liquid diagnostics, it is now more complex than ever for physicians to select the right test for the right patient. A key starting point is to recognize that different types of assays excel for different clinical intended uses — matching the performance characteristics of a test with the clinical context of each patient is necessary to appropriately inform medical decisions.

Cell-free DNA (cfDNA) was first discovered in 1948 (reference 3) and is now known to originate from many different sources including infectious organisms, fetal DNA during pregnancy, genomic DNA from white blood cells, and tumor cells. Tumor-derived cfDNA originating from necrotic and apoptotic tumor and deposited into peripheral circulation is known as circulating tumor DNA (ctDNA) and was first described about 40 years after the initial discovery of cfDNA (reference 4). The first studies relating disease burden and cfDNA levels were completed in the early 2000s, and in landmark studies conducted in 2008, investigators at Johns Hopkins University (Baltimore, MD) showed that ctDNA levels in patients with colorectal cancer change in response to changes in tumor burden (reference 5). Discrimination of ctDNA from normal DNA is achieved by the presence of mutations. However, due to the fact that ctDNA typically represents a very small fraction of cfDNA present in the blood, use as a biomarker for evaluating tumor dynamics requires a quantitative assay with high analytical and clinical sensitivity to characterize accurately the relatively low number of mutant ctDNA fragments in a sample.
Quantitative PCR (qPCR), next-generation sequencing (NGS), and digital PCR (dPCR) are the three most common technologies used for ctDNA analysis. Well-designed assays based on any of these methods can serve as useful diagnostic tools depending on the specific clinical needs of the patient.
Clinical evidence shows that very low frequency ctDNA mutations (<0.1% allele frequency in plasma) may have important clinical implications across a variety of different cancer types. This evidence continues to accumulate at a rapid pace (references 6-8). In these cases, ultra-high sensitivity is essential to ensure vital information is not missed so that patient samples are appropriately characterized.
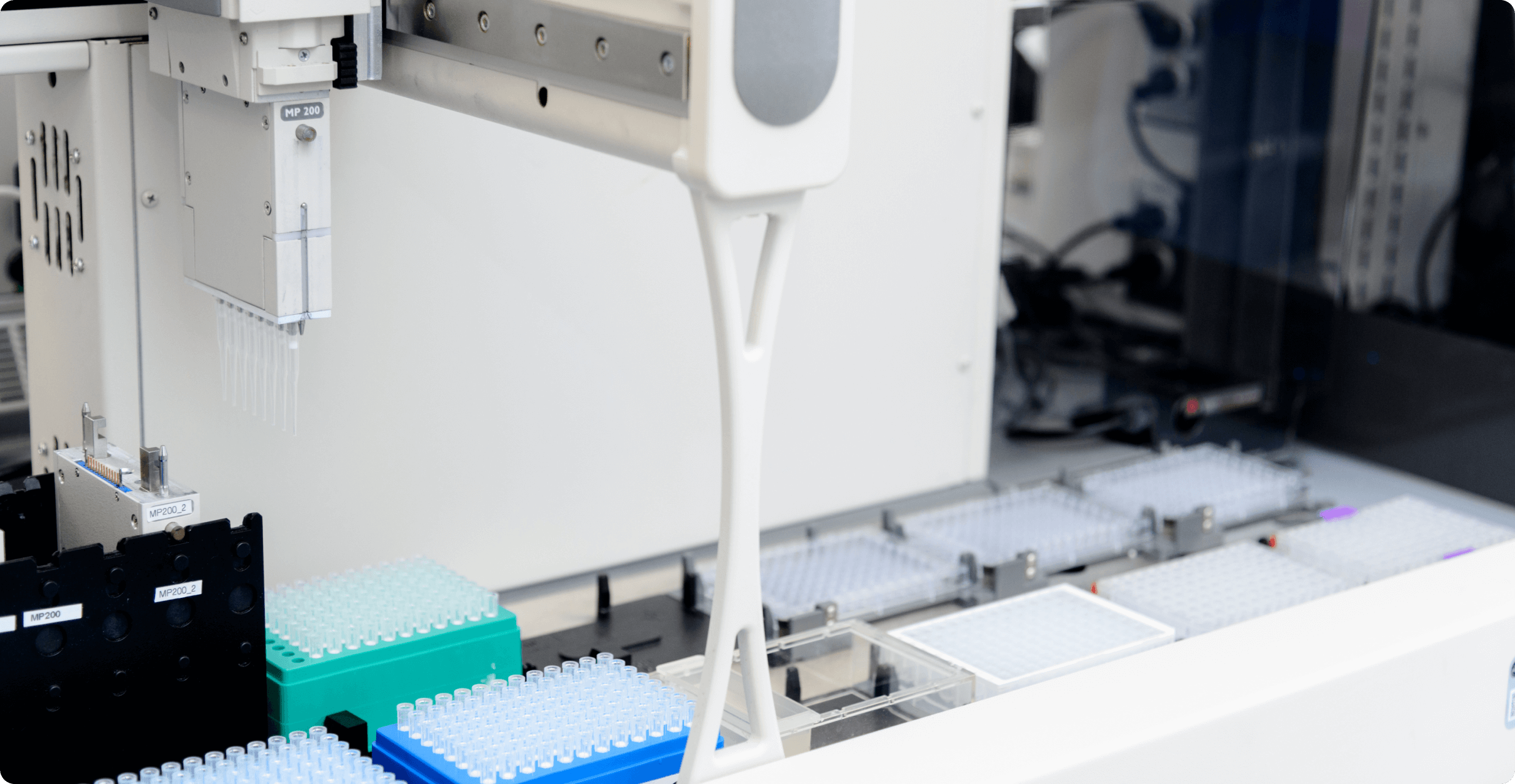
Sysmex OncoBEAM uses BEAMing technology (Beads, Emulsion, Amplification, Magnetics), a modified digital PCR method that interrogates millions of unique molecules within a sample to ensure detection of rare mutant molecules in the presence of many wildtype copies. The lower limit of detection is therefore consistent with low plasma mutant allele frequencies that are present for a significant proportion of cancer patients. Table 1 provides a comparison of analytical sensitivities for several leading ctDNA tests based on different technologies.

Table 1. Analytical sensitivities for several leading ctDNA tests.
Notes:
Acquired resistance to first-line tyrosine kinase inhibitors (TKI) for NSCLC patients who harbor epidermal growth factor receptor (EGFR) sensitizing mutations (exon 19 deletions, L858R point mutation) presents a common clinical problem. Resistance often develops after 10-12 months and is most commonly driven by an acquired mutation in EGFR, T790M, which presents in up to 60% of patients (references 14, 15). Third-generation TKIs such as osimertinib (approved by the FDA in Nov 2015) have been shown to be effective in patients with T790M-mediated resistance and disease progression.
Though tissue is the preferred sample type for EGFR analysis for NSCLC, obtaining a tissue biopsy in patients with advancing disease presents significant challenges. In addition to some patients being unwilling or unable to undergo secondary biopsy, the complication rate for intrathoracic biopsies is nearly 20% (references 16, 17). Furthermore, even if secondary biopsy is feasible, the combined turn-around time for tissue acquisition and subsequent molecular analysis can be too long, which can significantly delay the administration of appropriate therapy (references 18, 19). Tissue sampling in the setting of secondary resistance is further confounded by molecular heterogeneity, wherein T790M may be present in only a subset of tumor cells. Thus, sampling of a single region of single metastatic lesion by tissue biopsy may fail to capture the T790M cells that are driving resistance/ progression (reference 20).
Because ctDNA analysis is minimally-invasive, faster than tissue analysis, easily repeatable via additional blood draws, and may better represent disease heterogeneity, it is ideally suited for EGFR analysis for NSCLC patients who have progressed on first-line therapy. However, a ctDNA test used in this setting must have high analytical sensitivity since T790M may be present in a small number of tumor cells, as well as at low concentration in the blood. Most importantly, clinical data must demonstrate that the diagnostic test can be used to predict meaningful patient outcomes for second-line EGFR therapy.

Based on the study by Oxnard et al. using BEAMing (reference 21), NCCN guidelines now recommend plasma testing for EGFR T790M for NSCLC patients who have progressed on a first or second-generation TKI1. Equivalent clinical outcomes were observed between patients treated with osimertinib who were plasma-positive for T790M, and patients for whom T790M was detected via tissue analysis.

Importantly, for patients who were positive for T790M in tissue, the median mutant allele frequency for T790M detected in plasma by BEAMing was <1%, with a number of patients exhibiting the mutation at <0.1%. This is below the threshold for reliable detection for many other ctDNA assays, including broad NGS panels that excel at generating data across many genomic locations, rather than very high-resolution data focused on regions with established clinical significance.

Mutant allele fraction distribution for EGFR T790M, n=158 plasma samples
For 40% of samples, T790M was below 1% MAF and may not be reliably detected by conventional NGS testing. (reference 22)
Since guidelines recommend reflex to tissue testing if T790M is not detected in plasma, use of a highly sensitive ctDNA assay can aid clinicians to accurately and rapidly identify T790M mutations in patients and thereby avoid a tissue biopsy. It has been shown that BEAMing is able to reliably detect approximately 20-40% more T790M-positive patients compared to other, less sensitive methods, which translates directly into more patients who are spared from tissue biopsy and its associated complications (references 21, 23, 24).
While a highly sensitive assay may raise concerns of false positive results, OncoBEAM testing also demonstrates exquisite specificity. In a blinded profiling of 100 EGFR mutation-negative NSCLC patient plasma samples, BEAMing yielded no false-positive results (reference 25). This suggests that tumor heterogeneity, and not BEAMing assay performance, is the likely cause of discordance between T790M-positive plasma results and tissue-negative reference results.
Overall, use of a reliable and simple blood test decreases risk and cost for the greatest number of advanced NSCLC patients, and extends access to those who would otherwise not receive testing at all if tissue analysis were the only option available.

References: