Head and neck squamous cell carcinomas (HNSCC) develop from the mucosal epithelium in the oral cavity, pharynx, and larynx and are the most common malignancies that arise in the head and neck.1 Increasingly, tumors in the oropharynx are linked to prior infection with oncogenic strains of human papillomavirus (HPV), primarily HPV-16 and, to a lesser extent HPV-18 and others.2,3 HNSCCs of the oral cavity and larynx are primarily associated with tobacco-derived carcinogens, excessive alcohol consumption, or both, and are collectively referred to as HPV-negative HNSCC.4 The median age of diagnosis for non-virally associated HNSCC is 66 years, whereas the median age of diagnosis for HPV-associated oropharyngeal cancer is about 53 years.5
HPV-positive and HPV-negative HNSCC are two distinct diseases with different sites of origin, etiological agents, risk factors, and contributions to the development of oropharyngeal squamous cell carcinoma (OPSCC). The demographics, cause, and prevalence of HPV-positive and NPV-negative cancers are summarized in Table 1.
tumors in the oropharynx are linked to prior infection with oncogenic strains of human papillomavirus (HPV)
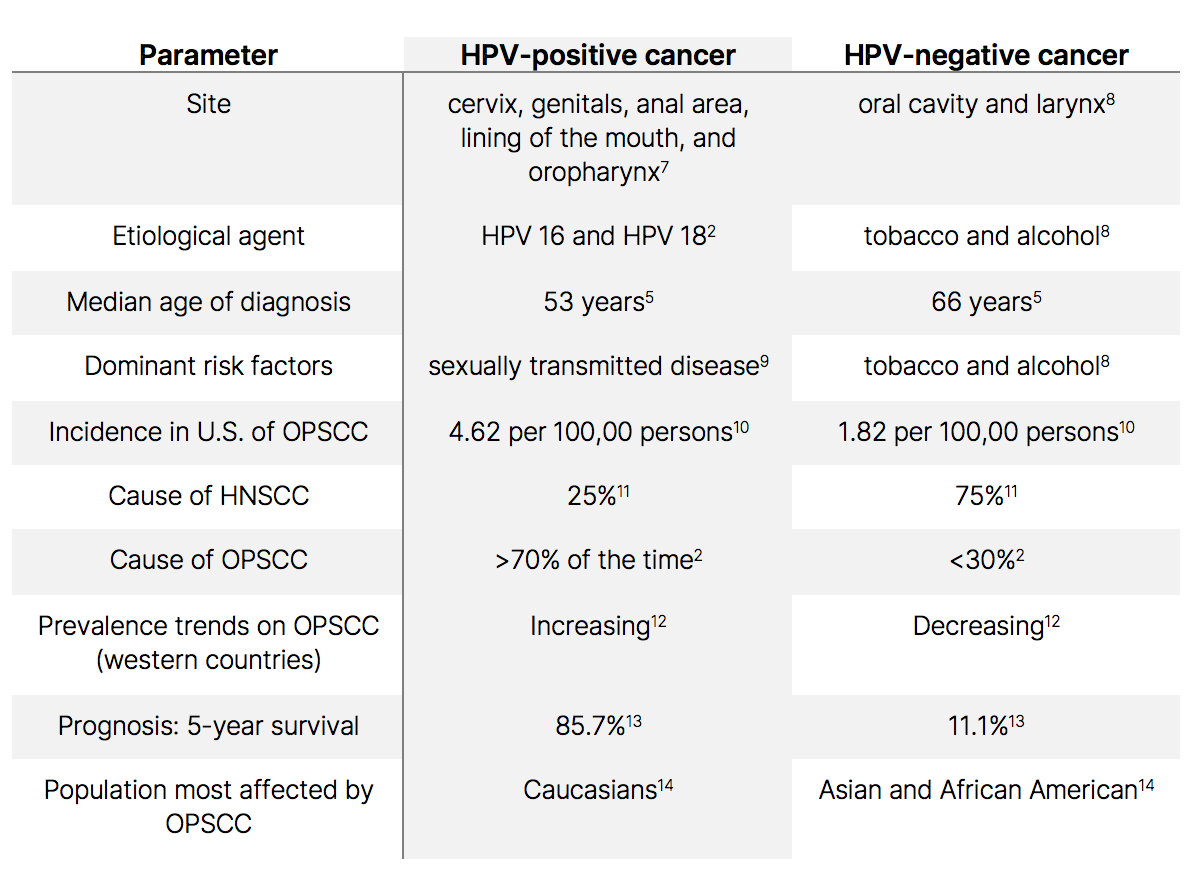
Table 1: Demographics, Cause, and Prevalence of HNSCC.
Whereas the incidence of smoking-related HNSCC continues to decline worldwide, that of HPV-positive HNSCC is on the rise.6 During 2007-2016, HPV-associated cancers increased by 2.1% per year on average, whereas cancers not associated with HPV decreased by 0.4% per year on average.6
HPV-positive and HPV-negative HNSCCs present with different molecular characteristics, immune landscapes, and clinical prognosis (Table 2) and lead to two fundamentally different diseases with distinct pathogenesis in terms of gene expression, tumor microenvironment (TME), and mutational burden.
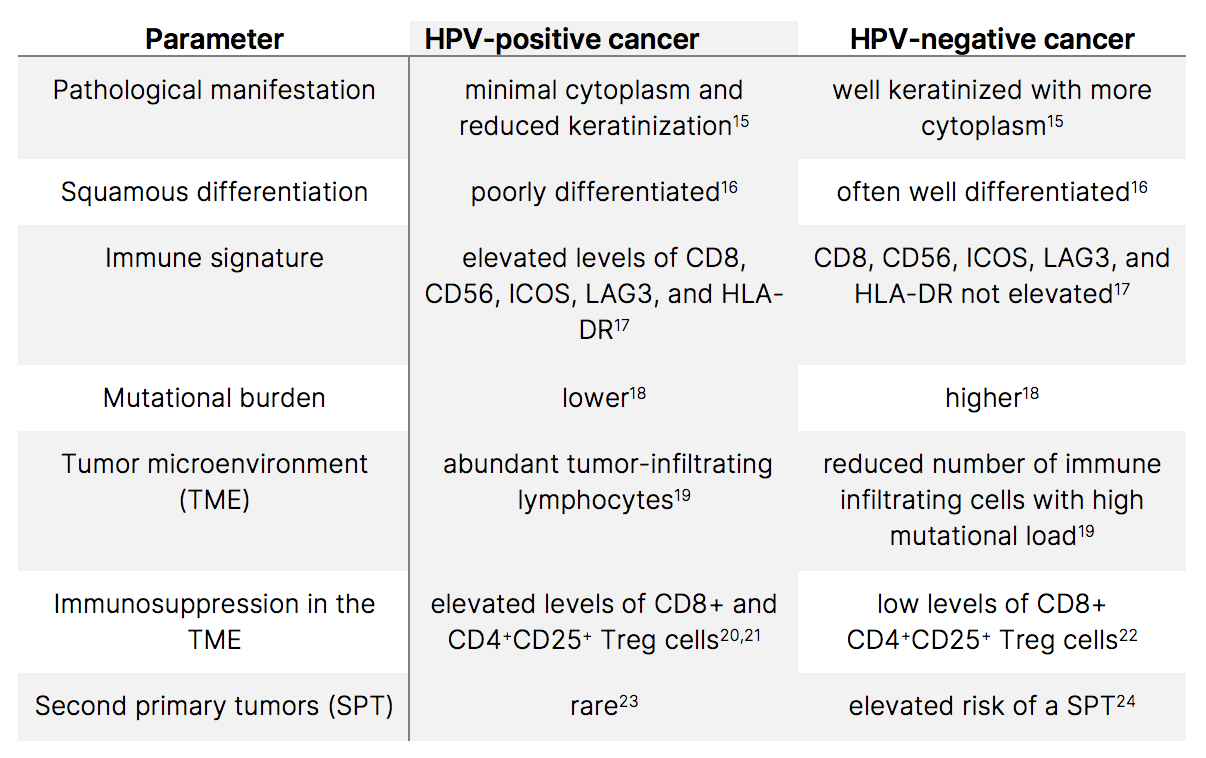
Table 2. Pathology and Disease Signature in HNSCC.
Genomic and epigenetic analyses reveal extremely high heterogeneity in HNSCC in terms of characteristic mutations, molecular signature, cellular phenotype, composition of TME, and immune landscape (Table 3).
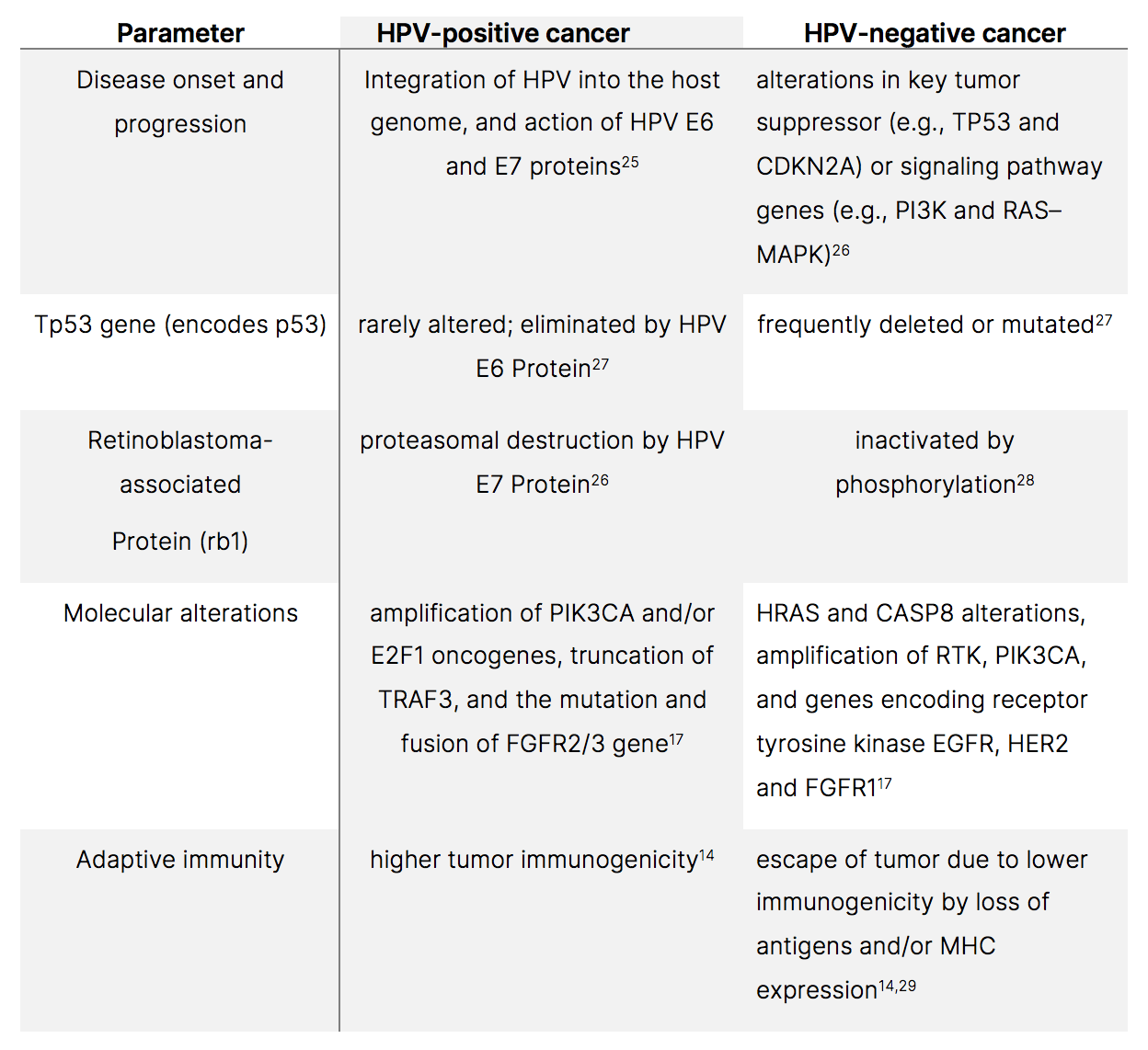
Table 3: Characteristic mutations in HPV-positive and HPV-negative HNSCC.
Various promising vaccine targets have been identified and treatment options employed for the treatment of HPV-positive and HPV-negative cancers with varying degrees of success (Table 4).
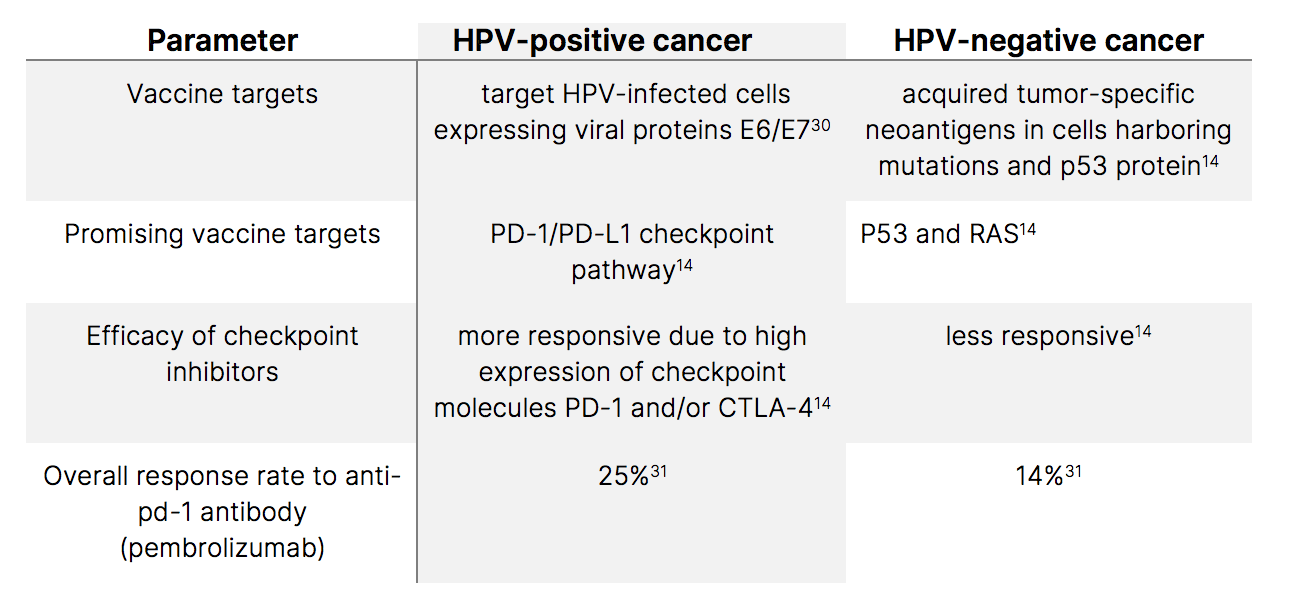
Table 4: Treatment options and targets.
Treatment personalization and de-escalation
According to Dr. Nishant Agrawal, Chief of Otolaryngology-Head & Neck Surgery UChicago Medicine, “We have seen a significant increase in the incidence of HPV-associated oropharyngeal cancer in relatively younger patients, with the median age of diagnosis in the 50s, even patients in their 30s.”32 He added that “Even at 2 years after radiation therapy, 15% of patients had grade 2 swallowing dysfunction and 8% had progressive dysphagia, so their swallowing is going to continue to get worse. Patients may also have chronic xerostomia. The dry mouth improves but it never gets back to 100%.”33 In contrast to patients with HPV-negative HNSCC, who have a five-year survival rate of about 25%-40%, patients with HPV-positive HNSCC fare much better with a disease-free survival rate of 85%-90% over five years. According to Dr. Agrawal, the better prognosis for HPV-positive patients suggests a need to de-escalate treatment while preserving survival.
References
- Stein, A.P. et al. (2015) Prevalence of human papillomavirus in oropharyngeal cancer: a systematic review. Cancer J. (21);138-46.
- Isayeva, T. et al. (2012) Human papillomavirus in non-oropharyngeal head and neck cancers: a systematic literature review. Head Neck Pathol. (6);S104-20.
- Michaud, D.S. et al. (2014) High-risk HPV types and head and neck cancer. Int J Cancer. (135);1653-61.
- https://pubmed.ncbi.nlm.nih.gov/33243986/
- Windon, M.J. et al. (2018) Increasing prevalence of human papillomavirus-positive oropharyngeal cancers among older adults. Cancer (124);2993-99.
- Ellington, T.D. et al. (2020) Trends in incidence of cancers of the oral cavity and pharynx – United States 2007-2016. Morb Morta Wkly Rep. (69);433-38.
- https://www.cancer.org/cancer/oral-cavity-and-oropharyngeal-cancer/causes-risks-prevention/risk-factors.html
- https://pubmed.ncbi.nlm.nih.gov/33243986/
- Gillison, M.L. et al. (2015) Epidemiology of human papillomavirus positive head and neck squamous cell carcinoma. J Clin Oncol. (33);3235-42.
- Mahal, B.A. et al. (2019) Incidence and Demographic Burden of HPV-Associated Oropharyngeal Head and Neck Cancers in the United States. Cancer Epidemiol Biomark Prev. 28(10);1660-67.
- Kazuhiro, K. et al. (2018) A Review of HPV-Related Head and Neck Cancer. J Clin Med Sep. 7(9);241.
- https://bmccancer.biomedcentral.com/articles/10.1186/s12885-022-09407-5
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5486734
- Canning, M. et al. (2019) Heterogeneity of the Head and Neck Squamous Cell Carcinoma Immune Landscape and Its Impact on Immunotherapy. Front Cell Dev Bio.l vol7. https://doi.org/10.3389/fcell.2019.00052
- Fakhry, C. et al. (2017) The prognostic role of sex, race, and human papillomavirus in oropharyngeal and nonoropharyngeal head and neck squamous cell cancer. Cancer (123);1566-75. Doi: 10.1002/cncr.30353.
- Pai, S.I. et al. (2009) Molecular pathology of head and neck cancer: implications for diagnosis, prognosis, and treatment. Annu Rev Pathol. (4);49-70.
- Keck, M.K. et al. (2015) Integrative analysis of head and neck cancer identifies two biologically distinct HPV and three non-HPV subtypes. Clin Cancer Res. (21);870-81. Doi: 10.1158/1078-0432.CCR-14-2481.
- Hanna, G.J. et al. (2018) Frameshift events predict anti-PD-1/L1 response in head and neck cancer. JCI Insight 3:98811. Doi: 10.1172/jci.insight.98811.
- Elpek, K.G. et al. (2014) The tumor microenvironment shapes lineage, transcriptional, and functional diversity of infiltrating myeloid cells. Cancer Immunol Res. (2);655-67. Doi: 10.1158/2326-6066.CIR-13-0209.
- Mandal, R. et al. (2016) The head and neck cancer immune landscape and its immunotherapeutic implications. JCI Insight 1: e89829. Doi: 10.1172/jci.insight.89829.
- Badoual, C. et al. (2013) PD-1-expressing tumor-infiltrating T cells are a favorable prognostic biomarker in HPV-associated head and neck cancer. Cancer Res. (73);128-38. Doi: 10.1158/0008-5472.CAN-12-2606.
- Hanna, G.J. et al. (2017) Defining an inflamed tumor immunophenotype in recurrent, metastatic squamous cell carcinoma of the head and neck. Oral Oncol. (67);61-69.
- Taberna, M. et al. (2017) Human papillomavirus-related oropharyngeal cancer. Ann Oncol. (28);2386-98.
- Coca-Pelaz, A. et al. (2020) The risk of second primary tumors in head and neck cancer: a systematic review. Head Neck. (42);456-66.
- Tomaic, V. (2016) Functional roles of E6 and E7 oncoproteins in HPV-induced malignancies at diverse anatomical sites. Cancers (8);95.
- Johnson, D.E. et al. (2020) Head and neck squamous cell carcinoma. Nat Rev Dis Primers. (6);92.
- The Cancer Genome Atlas Network [TCGA]. (2015) Comprehensive genomic characterization of head and neck squamous cell carcinomas. Nature (517) 576-82.
- Beck, T.N. et al. (2016) EGFR and RB1 as Dual Biomarkers in HPV-Negative Head and Neck Cancer. Mol Cancer Ther. 15(10);2486-97.
- Schreiber, R.D. et al. (2011) Cancer immunoediting: integrating immunity’s roles in cancer suppression and promotion. Science 331;1565-70.
- Skeate, J.G., et al. (2016) Current therapeutic vaccination and immunotherapy strategies for HPV-related diseases. Hum Vaccin Immunother. (12);1418-29.
- Seiwert, T.Y. et al. (2016) Safety and clinical activity of pembrolizumab for treatment of recurrent or metastatic squamous cell carcinoma of the head and neck (KEYNOTE-012): an open-label, multicentre, phase 1b trial. Lancet Oncol. (17);956-65.
- Dr. Nishant Agrawal, Chief of Otolaryngology-Head & Neck Surgery UChicago Medicine. Personal interview on 3/25/22.
- https:\\ascopost.com\\issues\\april-25-2017\\deintensifiying-treatment-of-hpv-positive-oropharyngeal-cancer-could-reduce-toxicity-while-maintaining-function-and-survival