Blog | Aug. 30, 2023
MRD in AML: the next step in fighting leukemia

The human immune system has the innate capability to recognize and eliminate cancer cells. However, cancers can grow progressively by evading recognition by the immune system or by suppressing its cytolytic activity. Cancer cells employ both mechanisms through various ways during the escape phase of immunoediting.1 Cancers can:
• minimize recognition through reduced antigen presentation
• develop resistant variants under selective pressure
• express proteins to boost resistance
• produce cytokines that suppress the immune system
• enhance angiogenesis
• suppress the immune system by expressing complementary ligands to immune checkpoints
Restoring the anti-tumor immune response is an important cancer treatment strategy. One of the most effective means to accomplish this has been to reverse immune tolerance by blocking the programmed death-1 (PD-1)/programmed death-ligand 1 (PD-L1) pathway. Hence, the development of immune checkpoint inhibitors (ICIs) is considered a revolutionary milestone in the field of immuno-oncology.2
Various mechanisms of immune evasion, including the PD-1/PD-L1 pathway, play a key role in the development and progression of HPV-positive HNSCC.3 In fact, the formation of HPV+ HNSCC is mainly due to PD-1/PD-L1 activation.3
PD-1 is a regulatory molecule expressed by activated T-cells. The binding of PD-1 to its complementary ligand, PD-L1, activates the signaling of PD-1 receptors which inhibits T-cell proliferation, cytokine generation and release, and antitumor activity.4 PD-1 expression is induced in many cell types in response to inflammation, caused by bacterial or viral infections, which leads to an increased expression of CD8+ T cells and CD4+ helper T cells to fight pathogens.5
PD-L1 is a transmembrane protein expressed in normal tissues to inhibit the activity of T-cells.6 The main role of the PD-1/PD-L1 pathway is to serve as “immune checkpoints” and prevent autoimmunity and excessive tissue destruction.4 While Interferon-gamma (IFN-γ) is considered the primary cytokine that triggers PD-L1 expression, several additional cytokines in the tumor microenvironment (TME), e.g., Interleukin-1⍺ (IL-1⍺), IL-10, IL-27 and IL-32 can upregulate PD-L1 expression.7
PD-1/PD-L1 binding regulates both the initiation and maintenance of T-cell tolerance and persistent antigen expression.8 It is responsible for a wide range of immune responses directed against tumors, pathogens, and self-antigens. Upregulation of PD-L1 interferes with proliferation of tumor-specific cytotoxic T cells and induces T cell exhaustion and apoptosis. PD-L1 limits the expansion of CD8+ T cells but does not affect their cytolytic activity.9
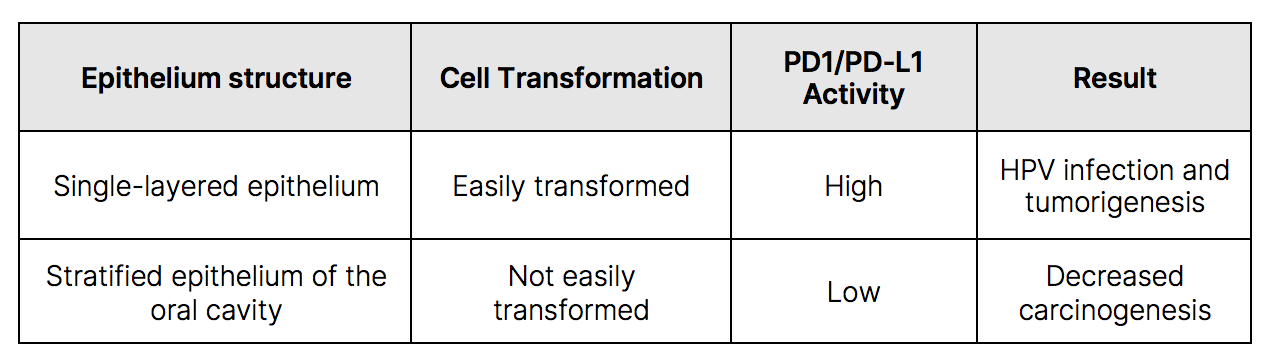
Microorganisms need suitable conditions to grow and thrive. Tonsils are gland-like structures in the back of the throat that help trap bacteria and viruses. They contain lymphocytes to protect the body from infections. Since they frequently harbor foreign debris and bacteria, their single-layered epithelium can easily uptake and incorporate exogenous material and alter the cells.10 These transformed cells can promote expression of PD-L1 which binds to PD-1 receptors inhibiting T cell activation and proliferation and allows cancer cells to evade immune checkpoints. This leads to persistent HPV infection and tumorigenesis. Furthermore, in tonsillar crypts, an enclosed biofilm of bacteria can form inside a matrix to protect HPV from the immune system.11 Conversely, the stratified epithelium of the oral cavity, which is also easily infected with HPV, is less susceptible to transformation and onset of carcinogenesis.10
PD-1 and Cytotoxic T-lymphocyte antigen 4 (CTLA-4) are two checkpoint molecules that suppress T-cell-mediated immune responses, leading to the development of tumors.12 PD-L1 is expressed on the surface of tumor cells and antigen-presenting cells in various solid tumors, including head and neck cancer.13 PD-1 is expressed on the surface of immune-related lymphocytes, such as T-cells, B-cells, and myeloid cells.14
Cancer immunotherapy is a specific method to eliminate cancer cells by enhancing the host immune system. Since PD-1/PD-L1 pathway is known to downregulate T-cell antitumor activity, monoclonal antibodies that inhibit either PD-1 or PD-L1 will reverse this immune suppression.15 This emerging paradigm in antitumor immunotherapy involves rejuvenating immunity by inhibiting the inhibitors that are responsible for silencing T-cells. It is believed that therapeutic interventions that overcome immune suppression may be more efficacious long-term than utilizing approaches that boost immunity, which are generally short-lived.9